Focused shock wave therapy (ESWT) in dermatology for the treatment of chronic wounds, accelerated healing of burns and open wounds

Shock waves induce healing processes
Focused shock waves create considerable tension in the tissue due to a sudden major increase in pressure. Receptors that monitor tissue integrity are subject to suprathreshold stimulation when exposed to shear, compressive and tensile forces (mechanotransduction). As a result, receptors stimulated in this manner trigger a reactive adapt-ation that affects the tissue’s characteristics.1
Highlights
- Stimulation of cell permeability
- Improved blood supply to the tissue through eNOS release
- Release of growth factors (e.g. VEGF)
- Enhanced cell regeneration through stem cell activation
- Antibacterial and anti-inflammatory effect
- Improved blood circulation through angiogenesis
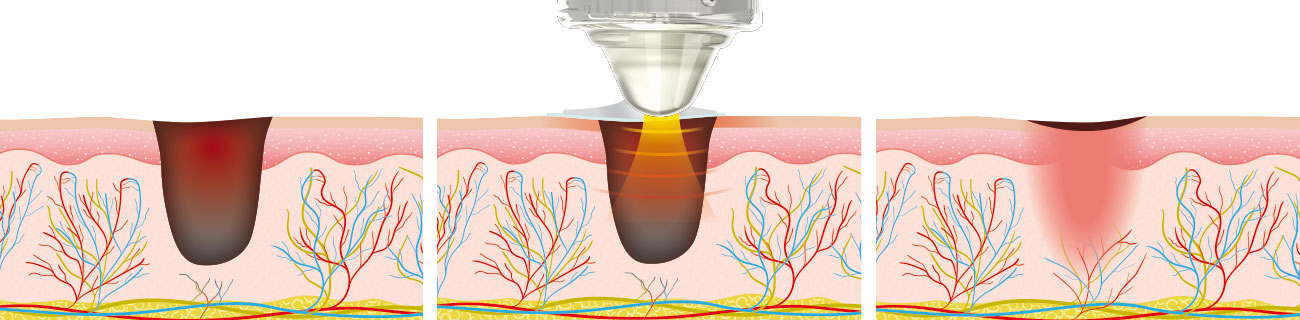
Schematic: Non-healing wound with impaired angiogenesis / Focused shock wave treatment of a non-healing wound / Extracorporeal Shock Wave Therapy stimulates angiogenesis
Focused shock wave therapy with C-ACTOR® handpiece
The DUOLITH® SD1 »ultra« boasts intuitive operation, an ergonomic handpiece and high-quality design. All essential treatment parameters (intensity/frequency) can be selected by using the buttons provided directly on the handpiece and are shown in the handpiece display. The C-ACTOR® handpiece is specially designed for near-surface treatments, making it ideal for use in dermatology and especially in wound healing.
Highlights
- C-ACTOR® handpiece specially designed for near-surface treatments
- Intensity and frequency control directly on the handpiece
- Different stand-offs to adjust the focal zone penetration depth (0 – 65 mm)
- Constant energy level (0.03 – 1.24 mJ/mm2)

Touch screen – The ideal add-on to the DUOLITH® SD1 T-TOP »ultra«
The optional 10" touch screen is connected with the shock wave system via a USB cable to provide valuable add-on features. Besides the additional device control, the touch screen offers patient management functionalities as well as treatment parameters recommended by experienced users and supported by images. These data and parameters can be retrieved and applied when required.
Highlights
- 10" touch screen (optional)
- Patient management system with treatment history
- Image-based treatment parameters
- Visible Body® digital anatomy atlas: macroscopic and microscopic 3D anatomy models
 Touch screen – Treatment parameters with images / Touch screen – Treatment example: wound healing / Visible Body® – Overview of the lymphatic system
Touch screen – Treatment parameters with images / Touch screen – Treatment example: wound healing / Visible Body® – Overview of the lymphatic system
Shock wave therapy for chronic wounds
Underlying diabetic diseases are often accompanied by chronic skin lesions. Several studies have shown that Extracorporeal Shock Wave Therapy (ESWT) significantly reduces healing times, improves and accelerates wound closure and achieves better functionality in the restored tissue.7,8,9 A review of randomized controlled trials revealed an almost doubled healing rate and an approximately 30% reduction in wound area when ESWT was used in addition to standard wound treatment. Moreover, the healing process was shortened by almost 3 weeks.10 Shock waves not only stimulate blood circulation but also induce the formation of new capillary blood vessels11. This is confirmed by the release of eNOS and VEGF proteins during shock wave therapy, whose metabolic effect enhances vascularization and thus wound closure12. In addition, a strong antibacterial13 and anti-inflammatory effect14 is observed as a result of ESWT.
Accelerated healing of burns and open wounds
In the treatment of burns and open wounds, it is important that the individual wound healing stages are initiated and completed as quickly as possible without disruptions. ESWT triggers a variety of mechanisms and clinical effects. The anti-inflammatory effect during the first wound healing stage is of partic-ular importance.16 It plays a key role in ensuring that wound closure progresses smoothly, especially following burns.17 The influence of ESWT on the initial inflammatory reaction has been demonstrated in both interleukin expression18 and macrophage activity.19 The use of ESWT from as early a stage as possible leads to a marked acceleration of the healing process and a significant reduction in the time to re-epithelialization20. In principle, shock wave therapy can be performed easily and largely without side effects at any stage of wound healing.
1 Huang, C. et al.: Trends in Molecular Medicine, 19(9):555-564, 2013.
7 Jeppesen, S. M. et al.: Journal of Wound Care, 25(11):641-649, 2016.
8 Moretti, B. et al.: BMC Musculoskeletal Disorders, 10:54, 2009.
9 Omar, M. T. et al.: Diabetes Research and Clinical Practice, 106(3):548-554, 2014.
10 Zhang, Li et al.: Wound Repair and Regeneration, 25(4):697-706, 2017.
11 Mittermayr, R. et al.: Annals of Surgery, 253(5):1024-1032, 2011.
12 Hayashi, D. et al.: Wound Repair and Regeneration, 20(6):887-895, 2012.
13 Gerdesmeyer, L. et al.: Ultrasound in medicine and biology, 31(1):115-119, 2005.
14 Moretti, B. et al.: BMC Musculoskeletal Disorders, 9(1):16, 2008.
16 Mittermayr, R. et al.: Wound Repair and Regeneration, 20(4):456-465, 2012.
17 Davis, T. A. et al.: International Wound Journal, 6(1):11-21, 2009.
18 Moretti, B. et al.: BMC Musculoskeletal Disorders, 9(1):16, 2008.
19 Sukubo, N. G. et al.: International Journal of Surgery, 24:124-130, 2015.
20 Mittermayr, R. et al.: Wound Repair and Regeneration, 20(4):456-465, 2012.

