Hostnik B. et al., 2025: Erectile Dysfunction in Diabetes Mellitus: A Comprehensive Narrative Review of Pathophysiology, Genetic Association Studies and Therapeutic Approaches.
Boštjan Hostnik 1 2, Gašper Tonin 2, Andrej Janež 1, Jasna Klen 2 3
1Division of Internal Medicine, Department of Endocrinology, Diabetes and Metabolic Diseases, University Medical Centre Ljubljana, Ljubljana, Slovenia.
2Faculty of Medicine, University of Ljubljana, Ljubljana, Slovenia.
3Division of Surgery, Department of Abdominal Surgery, University Medical Centre Ljubljana, Ljubljana, Slovenia.
Abstract
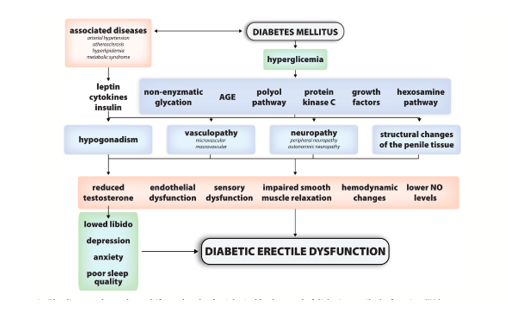
Introduction: Erectile dysfunction (ED) is a highly prevalent complication of diabetes mellitus (DM), significantly impairing quality of life and psychosocial well-being. The prevalence of ED is estimated to be over 3.5 times higher in men with diabetes mellitus compared to those without. The aetiology of diabetic ED is multifactorial, stemming from complex diabetes mellitus-related systemic changes. The pathophysiology of diabetic ED involves interacting pathways, including endothelial dysfunction, accelerated atherosclerosis, autonomic and peripheral neuropathy, structural penile changes, hormonal imbalances, and psychological factors.
Methods: A review of the literature was conducted to examine the pathophysiological mechanisms, genetic associations, and treatment modalities related to diabetic ED. Particular attention was given to studies exploring pharmacogenetics and emerging therapeutic interventions.
Results: Management is multimodal, including lifestyle changes, counselling, and pharmacological agents (primarily phosphodiesterase type 5 inhibitors (PDE5Is)), but treatment response varies. Genetic studies have identified associations between ED risk/severity and polymorphisms in several candidate genes, including NOS3 (G894T, T786C, VNTR), ARG1/ARG2 (influencing nitric oxide substrate availability), ACE (I/D polymorphism), AR (CAG repeat length affecting androgen sensitivity), and VEGF (promoter polymorphisms). Pharmacogenetic studies suggest that polymorphisms in NOS3, AR, and VEGF may predict response to PDE5Is or testosterone therapy, while ARG1/ARG2 variations might guide future arginase-targeted therapies. Emerging treatments like low-intensity shockwave therapy, platelet-rich plasma, gene therapy, and stem cell therapy show promise but require more robust evidence.
Conclusions: Diabetic ED is a complex condition driven by multiple pathophysiological mechanisms often influenced by an underlying genetic predisposition. Understanding the interplay between pathophysiology and genetics is crucial for developing personalised treatment strategies. While current therapies offer benefits, variability in response highlights the need for tailored approaches. Further research, especially large-scale pharmacogenetic studies and randomised controlled trials for emerging therapies, is essential to identify reliable biomarkers, optimise treatment selection, and improve outcomes for men with diabetic ED.
Endocrinol Diabetes Metab. 2025 Sep;8(5):e70099. doi: 10.1002/edm2.70099. PMID: 40960125; PMCID: PMC12441930


Comments 1
The article explores the complex relationship between diabetes mellitus (DM) and erectile dysfunction (ED), high-lighting its prevalence, causes, genetic factors, and treatment options focusing on pharmacogenetics and novel therapies.
Prevalence and Impact: Erectile dysfunction is notably more common in men with diabetes, being over three times more prevalent, which significantly affects their quality of life and mental health.
Aetiology of ED in DM: The causes of diabetic ED are multifactorial, involving various overlapping mechanisms, including:
- Endothelial dysfunction
- Accelerated atherosclerosis
- Autonomic and peripheral neuropathy
- Structural changes in the penis
- Hormonal imbalances
- Psychological factors
Basic Treatment Approaches: Management strategies are diverse and include:
- Lifestyle modifications
- Psychological counseling
- Pharmacological treatments, primarily phosphodiesterase type 5 inhibitors (PDE5Is).
However, the response to these treatments can vary significantly among individuals.
Genetic Associations: Various genetic studies identified links between erectile dysfunction and genes related to nitric oxide production, androgen sensitivity, and vascular endothelial growth factor (VEGF). Certain genetic polymorphisms may predict individual responses to ED therapies.
Emerging Therapies
Innovations such as low-intensity shockwave therapy, platelet-rich plasma, gene therapy, and stem cell therapy are discussed, with potential benefits noted but requiring further research for validation.
Low-Intensity Shockwave Therapy (LiSWT): LiSWT involves the use of acoustic waves to stimulate penile tissue. The therapy is thought to enhance blood flow and promote angiogenesis (formation of new blood vessels). Early studies suggest that it may improve erectile function in men with ED, including those with diabetes, though more extensive randomized controlled trials are needed to confirm its efficacy and safety.
Platelet-Rich Plasma (PRP) Therapy: PRP therapy involves injecting a concentration of platelets derived from the patient’s blood into the penis. The growth factors in PRP are believed to promote tissue healing and regeneration, potentially improving erectile function. Initial studies indicate some positive outcomes, but further research is required to establish standardized protocols and long-term effects.
Gene Therapy:Gene therapy aims to address the underlying causes of ED at the molecular level by delivering genes that promote endothelial function or enhance nitric oxide synthesis. While still largely in the experimental stage, this approach holds promise for long-term solutions to ED, especially in patients with underlying vascular issues.
Stem Cell Therapy: Stem cell therapy seeks to regenerate erectile tissues and improve vascular health by introducing stem cells into the penile area. Research is still in its infancy, but preclinical and early clinical trials show some potential benefits for men with diabetic ED. However, comprehensive studies are needed to assess safety, efficacy, and optimal methodologies.
Arginase-Targeted Therapies: Given the importance of nitric oxide in erectile function, therapies targeting arginase (which breaks down arginine—an important substrate for nitric oxide synthesis) may provide new treatment avenues. Genetic variations related to arginase metabolism could help tailor this approach to individuals, optimizing treatment responses.
Novel Pharmacological Agents: New medications that act on pathways involved in erectile function are being developed. This includes drugs that might affect nitric oxide pathways, hormonal modulation, or vascular function more directly.Research continues to explore the potential for these agents to provide alternatives for patients who do not respond to PDE5Is.
Conclusions
Diabetic ED is driven by an intricate interplay of pathophysiological factors and genetic predispositions. A personalized approach to treatment is advocated for better outcomes. The need for extensive pharmacogenetic research and randomized controlled trials is emphasized to enhance understanding and treatment efficacy.
Overall, the article stresses the importance of a comprehensive understanding of both the biological mechanisms and genetic factors influencing diabetic ED to improve personalized treatment strategies and patient outcomes.
The emerging therapies present exciting opportunities to improve erectile function in men with diabetes mellitus. While the initial findings are promising, there is a critical need for more robust clinical trials to evaluate the safety, effectiveness, and practicality of these treatments. Personalized medicine approaches, taking into account genetic predispositions and individual responses, will be crucial to advancing care in this field.
Jens Rassweiler